Mental Health in the age of prevention
An Interview with Dr. Péter Mendik, Medical Lead for Health Check at XUND.
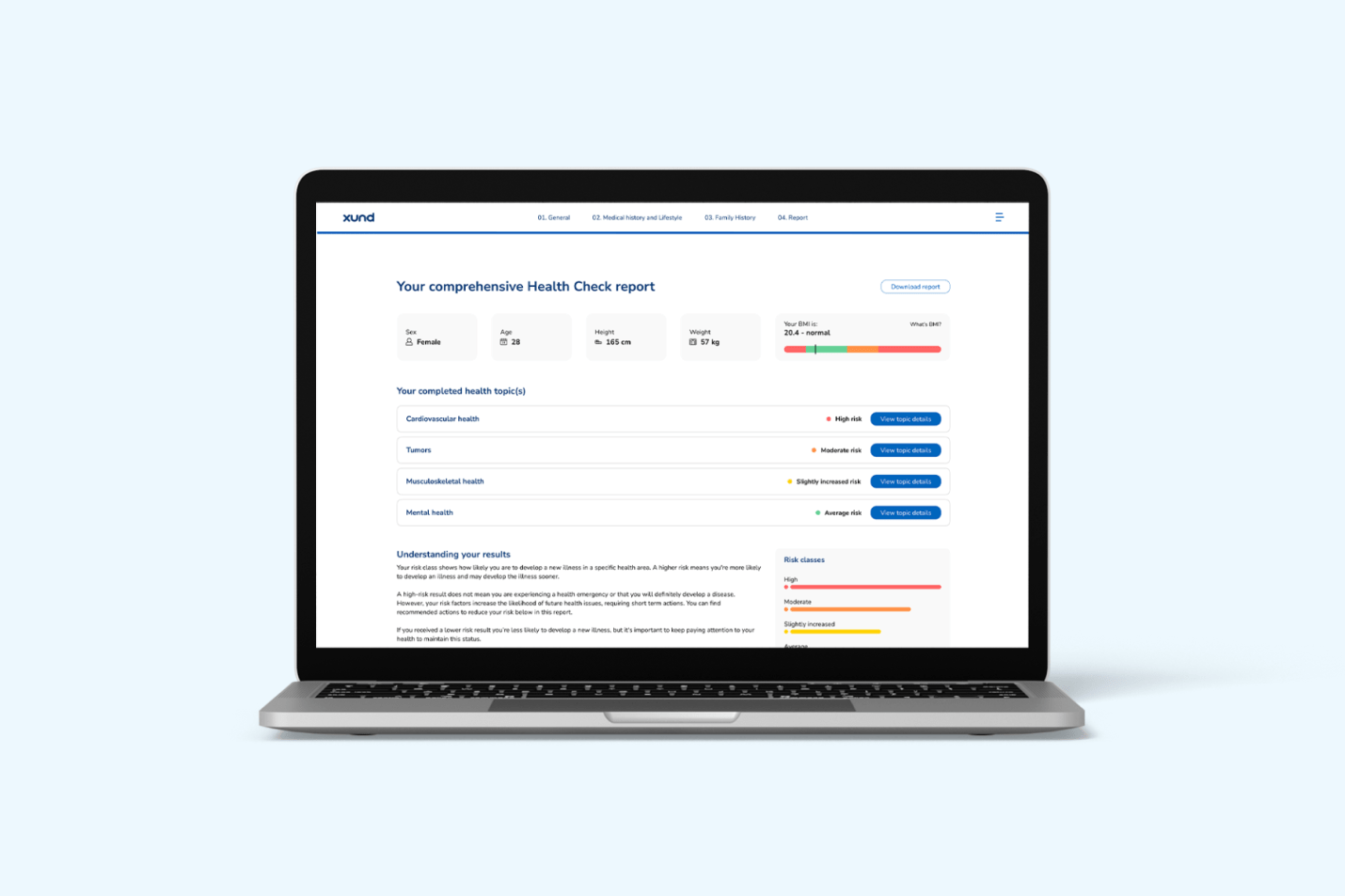
Mental health is increasingly recognized as a critical part of overall health, and a key driver of both clinical outcomes and healthcare costs. Dr. Péter Mendik, one of the clinical architects behind our medically certified Health Check, shares why prevention is the only sustainable path forward and how evidence-based, digital-first solutions can help health insurers and payers lead the way.

In your view, what are some of the biggest misconceptions people still have about mental health?
Péter: One of the most persistent misunderstandings is the idea that mental health problems are a sign of personal weakness. In reality, mental health is a mix of biological, psychological, and social factors – it’s much more complex than people often assume.
A genetic predisposition doesn’t necessarily mean someone will develop depression or anxiety. But when that vulnerability is combined with chronic stress, social isolation, or poor lifestyle habits, the risk increases significantly. And I think that understanding this complexity is essential because it shows us that there are many opportunities where we can step in and work on prevention.
Which early signs or risk factors should individuals – and systems – pay closer attention to?
Péter: Most mental health conditions don’t just appear out of nowhere. They usually develop slowly over time, often with subtle signs like trouble sleeping, difficulty concentrating, feeling more irritable, and losing interest in everyday activities.
What’s equally important is understanding protective factors: having a stable environment, supportive relationships, and healthy routines. Those may seem like personal things, but systems can and should play a role in enabling them. Digital tools like Health Check can help detect early warning signs across a population, long before individuals seek help.
In other words, systems shouldn’t wait for a crisis. When we give people the right insights and options, and we build infrastructure that lets us act early on, payers can shift the curve from reactive care to more proactive and preventive care.
Can you walk us through your role in shaping the Mental Health component of the new Health Check?
Péter: I led the medical development of the Mental Health topic, making sure it is clinically accurate, relevant, and based on the latest research. My responsibilities included defining the scope and overseeing the overall direction of the content. Developing a new health topic is an intensive process that requires a lot of deep research. Together with a team of medical experts, I spent a lot of time and effort identifying key risk factors and digging into areas that are more complex or ambiguous, often through detailed discussions and reviewing literature.
What medical guidelines or evidence were used for the development of the Mental Health topic?
Péter: We worked with high-quality, peer-reviewed sources:
- Clinical guidelines from national and international associations (e.g., DGPPN, NICE, WHO)
- Meta-analyses and systematic reviews from randomized controlled trials (RCTs)
- Validated tools from psychiatric and psychological care, adapted for preventive use
We also validated the health topic against a subset of the UK Biobank, a large-scale biomedical database of over 500,000 individuals. That level of validation allows us to assess not only scientific accuracy but also how well our Health Check performs across diverse, real-world populations.
How did you ensure that the Mental Health assessment is not only clinically sound but also feels empathetic and supportive for users?
Péter: For us, medical accuracy and user experience go hand in hand. A solution can only make a difference if people are willing to engage with it. That’s why we co-develop Health Check with colleagues from other departments, including experts in user-facing content and health literacy. One of our team members, for example, has a background in medical sociology and focuses exclusively on ensuring our language is clear, accessible, and empathetic. The result is something that feels respectful, intuitive, and non-stigmatizing.
We also iterate regularly based on real user feedback. Health Check is not a static tool, and we adjust it on the go as we learn more and as users' needs change.
What does it mean for a digital mental health assessment to qualify as a certified medical device, and why does that matter for insurers and healthcare providers?
Péter: Health Check is a certified class I medical device under the EU Medical Device Regulation (MDR). This means that the product is safe, effective, and backed by clinical evidence.
For payers, this matters for two reasons: First, it offers legal and regulatory clarity. Because the API itself is the medical device, Health Check can be offered to insurance members as a medically validated product, without requiring payers to take on the role or liability of a medical device manufacturer. And second, the certification guarantees clinical accountability. Payers can be confident that the services they offer are evidence-based and medically sound.
Mental health data is especially sensitive. How do you ensure user data is secure and handled responsibly?
Péter: Our Data Protection Officers know more about the specific compliance, but I can say with certainty that our processes are designed around data minimization. We only collect what is necessary to generate meaningful risk assessments, and data is shared with our clients in aggregated formats, never individually.
Our systems are fully GDPR-compliant and undergo both internal and external review. In mental health especially, privacy has to be foundational.
What makes this approach to mental health prevention scalable for large populations, such as insured members?
Péter: Three key factors:
- Member health status: Health Check identifies early mental health risks across broad populations, enabling targeted, preventive outreach.
- Digital reach: As a web-based product, it’s accessible anytime & anywhere, allowing insurers to engage members beyond office hours and without geographic limitations.
- Ease of deployment: As a web-based solution, it can be deployed quickly and at scale, without requiring deep integration into existing ecosystems.
For insurers and payers, this means mental health prevention becomes digitally scalable, supporting large populations efficiently.
How can health insurers or payers integrate the Mental Health Check into existing care or prevention pathways?
Péter: Health Check was designed to plug in where it’s needed. It can be offered during onboarding, as part of preventive outreach, or integrated with mental health partners for stepped care.
It is also customizable, so it fits neatly into existing care journeys or prevention frameworks. For payers, this is a chance to move from reactive treatment to proactive prevention.
If you could share one piece of advice for anyone wanting to take better care of their mental health, what would it be?
Péter: I could mostly come back to the earlier points:
Don’t wait for symptoms to become severe and act early. Mental health benefits most from prevention. Try to create an environment where you can feel safe and don’t be afraid to address problems in your life.
And this isn’t just a message for individuals. Systems have the power to embed prevention where it matters: in everyday routines, in digital access points, and in the way we measure health.
It is important to remember that mental health doesn’t exist in isolation. It’s shaped by how we live, work, and connect. If we take that seriously, we can reduce the burden of illness.